

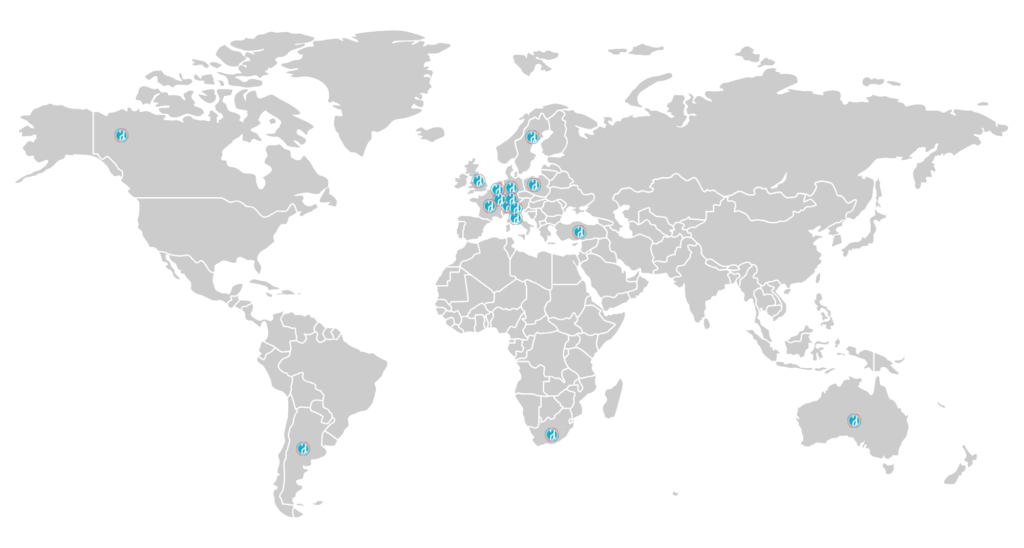
EA is a rare congenital condition, and with rarity often comes isolation. For over 40 years, family-led support groups around the globe have been stepping in to bridge that gap — offering community, guidance, and advocacy. EAT unites these efforts on an international level.
We exist to:
Share knowledge across borders
Raise awareness of EA globally
Improve care and long-term support for those affected
Promote collaboration between families, medical professionals, and researchers
As a charitable, non-profit organization, EAT works exclusively in the interest of the EA community. All member groups operate with the same non-commercial principles.
At EAT, we envision a world where every person born with Esophageal Atresia (EA) — no matter where they live — has access to:
Accurate diagnosis and early treatment
Consistent, high-quality long-term care
Empowered families and patients who feel seen, heard, and supported
A strong, connected global community working together to improve outcomes
We believe that by uniting families, healthcare providers, researchers, and advocates across borders, we can build a future of better health, understanding, and hope for everyone affected by EA and related conditions.
EAT is committed to driving progress — not just in medical care, but in the everyday lives of the people we serve.

Whether you’re a national support group, a healthcare provider, or a family looking for connection — EAT welcomes associate members from every corner of the world.
We are proudly headquartered in Stuttgart, Germany, where we are formally registered as a non-profit organization (Registration Number: VR 720961, Amtsgericht Stuttgart).

Our key areas of action include:
While support systems vary from country to country, many of the challenges are strikingly similar:
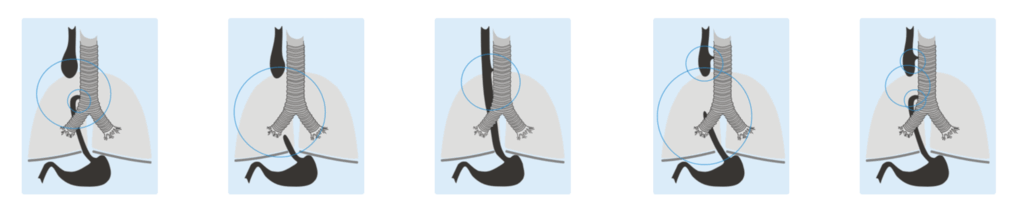
Esophageal Atresia (EA) and Tracheoesophageal Fistula (TEF/TOF) are rare congenital condition that affect newborns. These conditions involve abnormalities in the esophagus(feeding tube) and trachea (windpipe), which can cause serious difficulties with swallowing and breathing.
What Is Esophageal Atresia?
Esophageal Atresia occurs when the esophagus fails to develop properly during pregnancy. Instead of forming a continuous passage from the mouth to the stomach, the esophagus ends in a blind pouch — meaning food and liquids cannot reach the stomach. This makes feeding impossible without medical intervention.
How Common Is EA/TEF?
EA affects approximately 1 in every 2,400 to 4,500 live births worldwide. Many babies with TEF are also born with EA — in fact, around 90% of infants with TEF also have EA.
What Is Tracheoesophageal Fistula?
Tracheoesophageal Fistula is a condition where there is an abnormal connection (or “fistula”) between the esophagus and trachea. This allows food or stomach contents to enter the airway, which can lead to:
Living with Esophageal Atresia (EA) is not just a medical condition — it’s a journey that begins before birth and continues throughout life.
From prenatal diagnosis to adulthood and beyond, each stage presents its own challenges, milestones, and moments of hope. Whether you’re a parent, patient, or healthcare provider, understanding this journey can make a world of difference.
Explore the timeline below to learn what to expect at each step — and discover how support, information, and community can help you navigate it with confidence.
The EAT Federation works with a diverse community of individuals and organizations impacted by Esophageal Atresia (EA).
Each group has unique needs — and we tailor our support to ensure no one faces this journey alone.
Below, you’ll find a summary of the key audiences we serve, their specific challenges, and how EAT helps respond to those needs through collaboration, information, and advocacy.
Living with Esophageal Atresia (EA) is not just a medical condition — it’s a journey that begins before birth and continues throughout life.
From prenatal diagnosis to adulthood and beyond, each stage presents its own challenges, milestones, and moments of hope. Whether you’re a parent, patient, or healthcare provider, understanding this journey can make a world of difference.
Explore the timeline below to learn what to expect at each step — and discover how support, information, and community can help you navigate it with confidence.

Sometimes, EA is detected during pregnancy through routine ultrasounds.
While a prenatal diagnosis can be overwhelming, early awareness allows families to access accurate information, prepare emotionally, and connect with specialists before birth.

After birth, EA is typically confirmed when feeding difficulties arise or through routine checks in the neonatal unit.
This is a critical moment that requires rapid action, expert care, and compassionate support for the family.

Surgical repair usually happens within the first few days of life.
The type of procedure depends on the individual anatomy of the baby. Though complex, surgery is a vital first step toward recovery and long-term health.

The days and weeks after surgery are a time of careful monitoring and healing.
Babies often remain in intensive care while medical teams ensure recovery is on track and complications are managed quickly.

Going home is a major milestone — but it also brings new responsibilities.
Families take over daily care, often involving feeding tubes, medications, and follow-up appointments, all with continued guidance from their care team.

Learning to eat by mouth can be a gradual and emotional process.
Children may face challenges with swallowing, reflux, or food aversions. Nutrition support and patience are key during this stage.

Starting school introduces new routines and social environments.
Parents often collaborate with teachers and health professionals to ensure the child’s needs are understood and accommodated, both medically and emotionally.

Regular follow-ups help monitor a child’s growth, development, and long-term health.
These appointments are essential for managing issues like strictures, reflux, or respiratory symptoms that can arise over time.

As children grow into teens and young adults, their care needs evolve.
Transitioning from pediatric to adult care requires planning, education, and support — empowering young people to take more responsibility for their health.

Moving out and gaining independence is a big step.
Young adults with EA still benefit from ongoing medical support, especially as they begin to manage their own healthcare and connect with peers who share similar experiences.

Even in later stages of life, EA-related issues can persist.
Long-term follow-up, access to experienced healthcare providers, and staying informed help maintain quality of life at every age.

Follow us on Social Media:
Important links:
© Copyrights 2025 – EAT Federation

We are conducting a global survey to better understand the real experiences, challenges, and needs of people living with Esophageal Atresia (EA) worldwide.
Your participation is essential to ensure that the patient and family perspective is heard by international medical experts and reflected in future care and support.
Please note: one questionnaire should be completed for each person living with EA, by the family or caregivers if applicable.
*For people living with EA and parents/caregivers
*Takes less than 10 minutes
*Every response helps strengthen our global community
Together, we can raise EA awareness and create real impact.
Take part and make a difference!